The New England HIMSS Annual Spring Conference held on May 16, 2019 at Gillette Stadium included a range of speakers who directly—or indirectly—spoke about the uses of data in healthcare. Here are my highlights, seen through my (permanent) #healthdata lens.
Richard Parker, MD, Chief Medical Officer, Arcadia, kicked off the day describing how Arcadia strives to identify the most “actionable” patients from the most “impactable” segments of the provider’s population.
Dr. Parker described the predictive analytics process in broad strokes and referred to the foundational step of aggregating data—including claims data, EHR data, medications data—as “not easy” and that they want all the data they can get their hands on to improve their predictive models. I asked him for more detail on the biggest challenge in aggregating & cleaning the data inputs, the “non-sexy” elements of data science as I called it. For Arcadia, access to EHR data is granted by clients that provide the data feeds and who are provided access to the curated and cleansed aggregated data, as well as the outcomes of the modeling exercises.
Dr. Richard Parker
Micky Trapathi, President and CEO, Massachusetts eHealth Collaborative, described interoperability as a “dimmer switch” rather than an “on/off switch”. To put it in my words, interoperability is not a thing or an inherent property of a data set. Rather, it requires common data standards and communications specifications between the parties that want to exchange data. The degree of interoperability depends on how highly specified the data set is and how well the parties exchanging data follow the same specifications.
For the present, FHIR does a good job in defining standards and specifications for limited data items and use cases, but we have a long way to go before data exchange is optimized for a wide range of use cases. Tripathi illustrates the current state with a cube diagram with only a portion of the lower left-hand space completed.
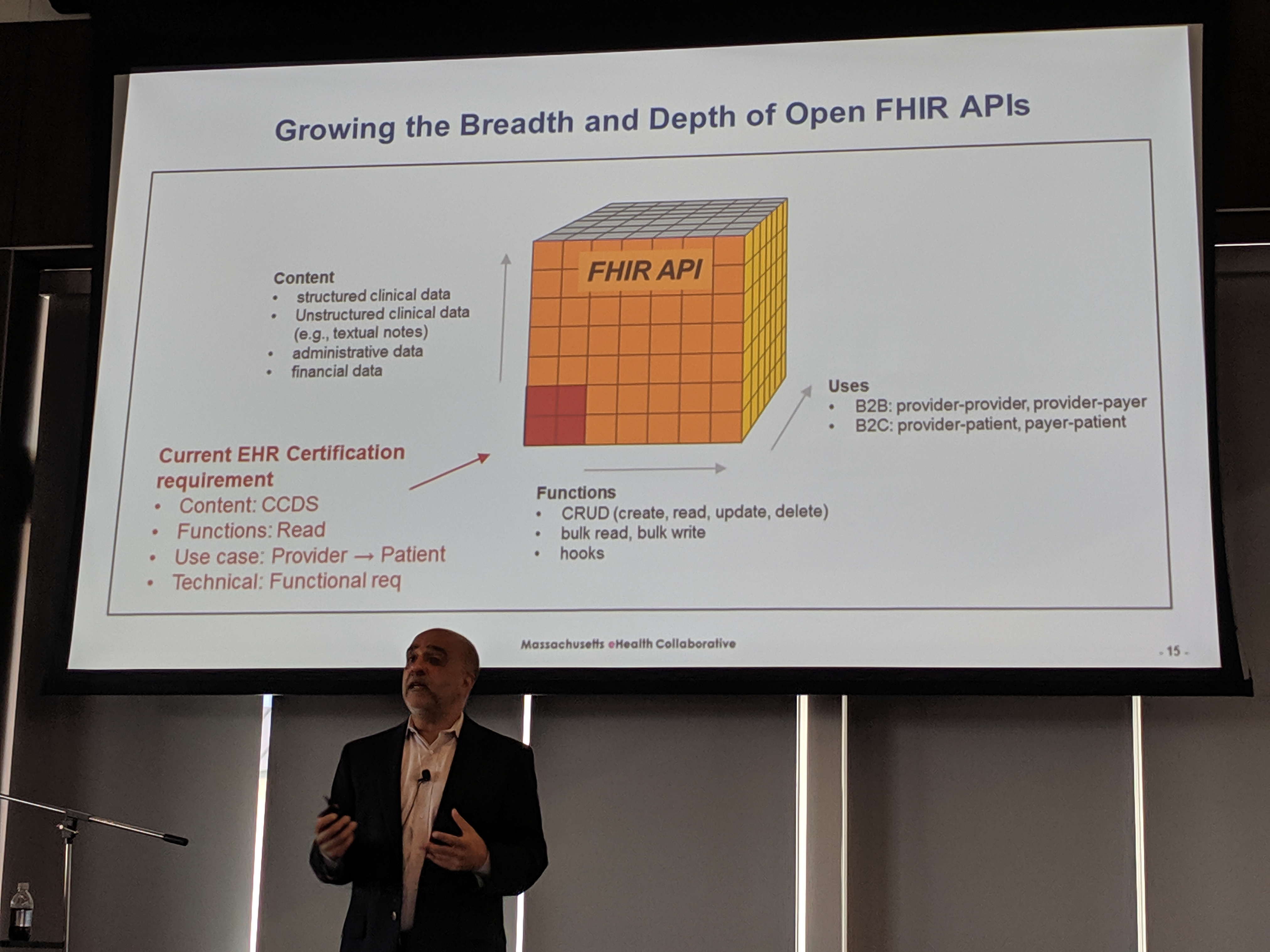
Micky Tripathi
Larry Garber, MD, Medical Director for Informatics, Reliant Medical Group, illustrated how Reliant has created a working ecosystem that includes a larger set of data exchange scenarios than those required by current regulations. Reliant has an early mover advantage, as pointed out by my friend Matt Fisher, who has good knowledge of Reliant’s model & history.
@Matt_R_Fisher
Keys to #EMR success from @GetReliant Dr. Garber. Comes from lengthy experience that predates #regulatory forced adoption. Arguable clear advantage. #NEHIMSS
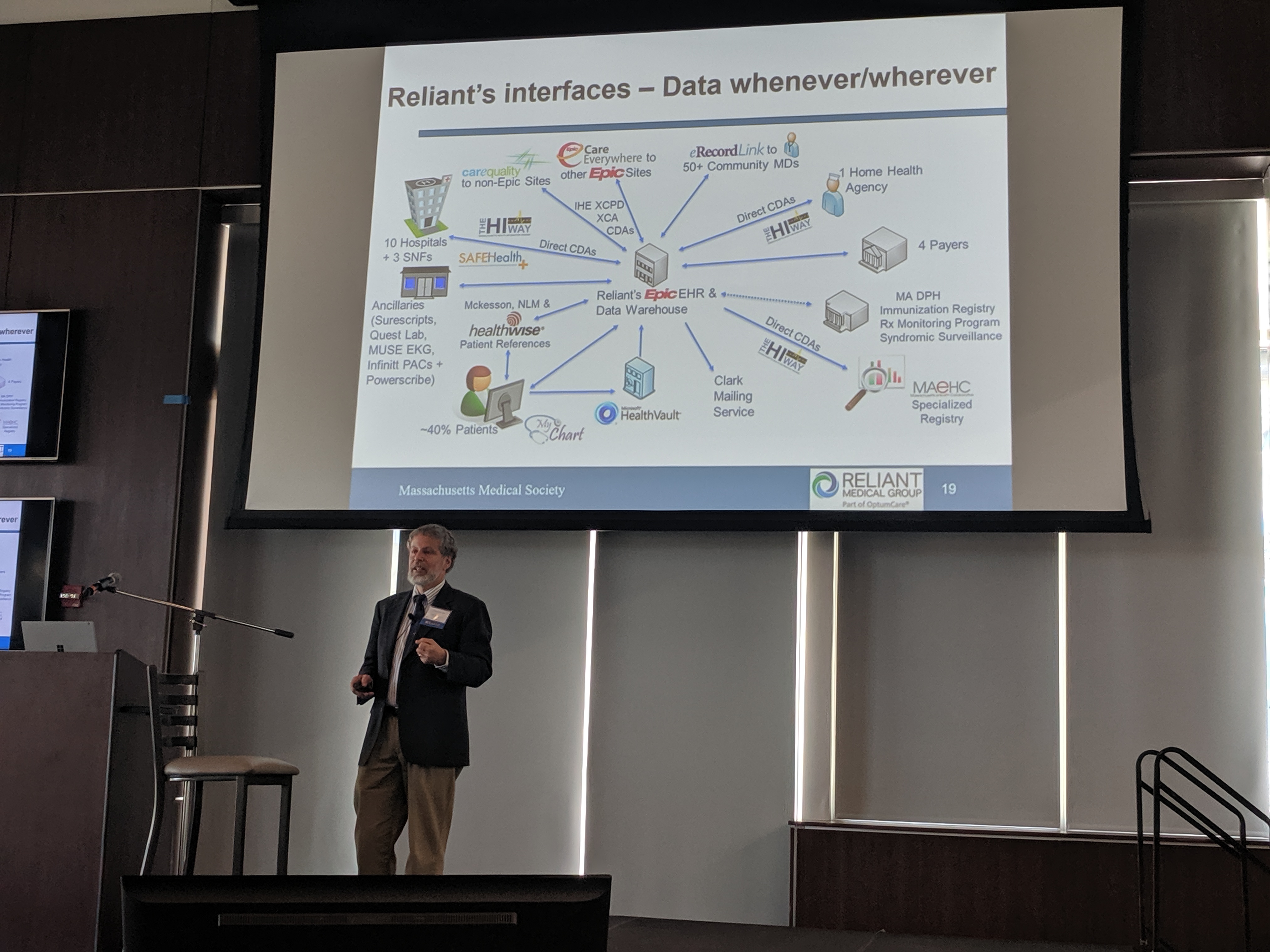
Dr. Larry Garber
My takeaway from the CIO panel: hospitals and physician practices are still struggling with understanding the value of data for their everyday purposes of treating patients. However, when shown how aggregated data can be applied in specific areas, such as identifying when a patient needs follow-up or what group of patients need to be prioritized, the value becomes self-evident. Presumably, the ability to recognize the value of data will improve after clinicians gain experience with early use cases that demonstrate improved efficiency and outcomes.
What about the downside of high-value data?
Juhan Sonin, Creative Sandpaper, Director of GoInvo and Lecturer, MIT, who envisioned the home-based healthcare center of the future when he spoke at NEHIMSS two years ago, tackled some of the problems associated with extracting value from health data when access is restricted. Furthermore, with so much data being generated by all sorts of devices and aggregated by firms that provide profiles and screening criteria to marketers, we’re deep in the age of surveillance. Providing patients/individuals with control or ownership of their own health data is the only way to transform the age of surveillance into a net positive for individuals according to Sonin (and I agree).
Health Content Advisors’ Recap
In the digital age, where all content is data, we often hear comparisons that “data is the new oil” or “data is the new water”. The Lancet even published an article recently, “Data is the New Blood”. I have two disclaimers to add to those proclamations, both of which were reinforced at the New England HIMSS spring conference:
I) If data is the new oil, then we’re still at the stage of figuring out how to refine the data;
II) Data doesn’t have value until someone uses the data.
I’d like to thank the New England HIMSS chapter and the volunteers who put together an outstanding program again this year. See more info on the program, speakers, presentations and sponsors here:
http://ne.himsschapter.org/event/new-england-himss-annual-spring-conference-save-date.
Finally, a special shout-out to E Ink, who not only sponsored breakfast but whose prize I won at the end-of-day raffle. I love my electronic paper wall clock!